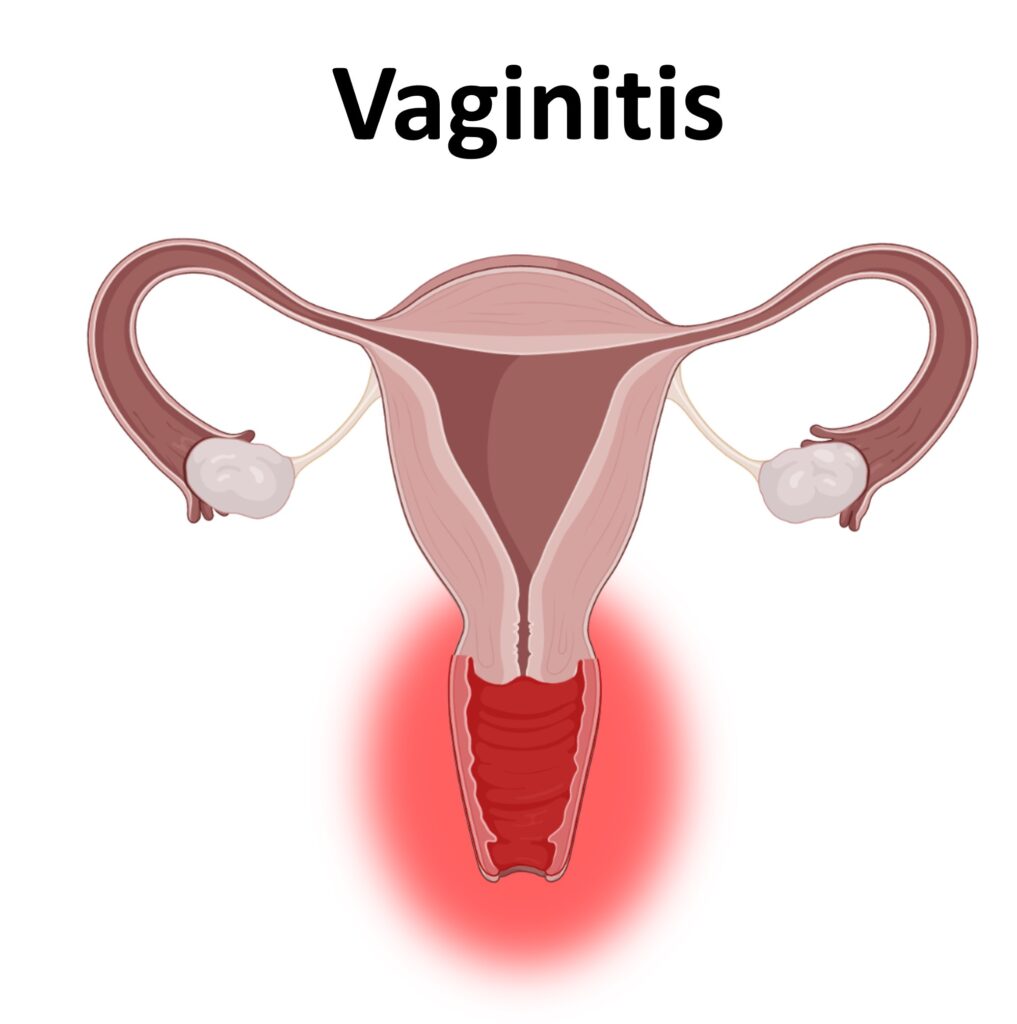
Vaginitis is a common condition that affects millions of women worldwide. It refers to inflammation of the vagina, which often results in discomfort, abnormal discharge, itching, or pain. Although it is usually not serious, vaginitis can significantly impact quality of life if left untreated. This comprehensive guide will walk you through what vaginitis is, its different types, causes, symptoms, diagnosis, treatment options, and preventive strategies.
What is Vaginitis?
Vaginitis is an umbrella term for various conditions that cause infection or inflammation of the vagina. The most common types include:
- Bacterial Vaginosis (BV)
- Yeast Infections (Candidiasis)
- Trichomoniasis
- Non-infectious Vaginitis (Atrophic or Allergic)
Each type has distinct causes, symptoms, and treatments, making it essential to identify the specific form accurately.
Common Types of Vaginitis
Bacterial Vaginosis (BV)
BV is the most common cause of vaginitis in women of reproductive age. It results from an imbalance in the vaginal bacteria, where harmful bacteria outnumber the beneficial ones like Lactobacillus.
Symptoms:
- Thin gray or white discharge
- Fishy odor, especially after intercourse
- Mild itching or burning
Causes:
- Multiple or new sexual partners
- Douching
Yeast Infections (Candidiasis)
Caused by an overgrowth of the fungus Candida, particularly Candida albicans.
Symptoms:
- Thick, white “cottage cheese”-like discharge
- Intense itching
- Redness and swelling
Causes:
- Antibiotics
- Hormonal changes (e.g., pregnancy)
- Uncontrolled diabetes
Trichomoniasis
A sexually transmitted infection caused by the parasite Trichomonas vaginalis.
Symptoms:
- Frothy, greenish-yellow discharge
- Bad odor
- Itching, burning, and soreness
- Pain during urination or sex
Non-Infectious Vaginitis
Triggered by irritants or allergens such as soaps, tampons, or hormonal changes.
Symptoms:
- Burning or itching
- Dryness
- Pain during intercourse
Common in: Postmenopausal women due to decreased estrogen levels.
Causes and Risk Factors

Understanding what causes vaginitis is key to both treatment and prevention.
Common Causes:
- Disruption of vaginal flora
- Sexual activity
- Poor hygiene
- Hormonal imbalances
- Use of irritating products
Risk Factors:
- Multiple sexual partners
- Frequent douching
- Uncontrolled blood sugar
- Use of corticosteroids or antibiotics
Diagnosing Vaginitis
Diagnosis involves a thorough medical history, physical examination, and lab tests.
Steps for Diagnosis:
- Pelvic examination
- pH test of vaginal fluids
- Microscopic evaluation
- Cultures or DNA testing
Your healthcare provider will determine the specific cause and recommend an appropriate treatment.
Treatment Options for Vaginitis
Medical Treatments
1. Bacterial Vaginosis:
- Oral or topical antibiotics (e.g., metronidazole or clindamycin)
2. Yeast Infections:
- Antifungal creams or suppositories (e.g., miconazole, fluconazole)
3. Trichomoniasis:
- Oral metronidazole or tinidazole (both partners should be treated)
4. Atrophic Vaginitis:
- Estrogen creams, tablets, or rings
Home Remedies (with caution)
- Yogurt with live cultures
- Tea tree oil suppositories (consult doctor first)
- Avoiding irritants (fragranced soaps, tight clothing)
Note: Always consult a healthcare provider before trying any home remedy.
Prevention Tips
Preventing vaginitis often involves maintaining good hygiene and adopting healthy habits.
Daily Practices:
- Wear breathable cotton underwear
- Avoid tight clothing
- Wipe from front to back
- Avoid douching
- Use mild, unscented soap
Sexual Health:
- Practice safe sex (use condoms)
- Urinate after intercourse
- Limit the number of sexual partners
Vaginitis in Special Populations
During Pregnancy
Hormonal changes increase susceptibility to yeast infections. Treatment must be pregnancy-safe.
In Postmenopausal Women
Declining estrogen levels can lead to atrophic vaginitis. Estrogen therapy may help relieve symptoms.
In Children
Often results from poor hygiene or irritants. Pediatric evaluation is essential.
When to See a Doctor
Seek medical attention if you experience:
- Persistent or severe symptoms
- Recurring infections
- Painful urination or intercourse
- Vaginal bleeding not related to menstruation
Early diagnosis helps prevent complications and improves quality of life.
Complications if Left Untreated
- Pelvic Inflammatory Disease (PID)
- Increased risk of STIs
- Pregnancy complications (in case of BV or trichomoniasis)
- Chronic discomfort or scarring
Frequently Asked Questions (FAQs)
Q: Can I get vaginitis without being sexually active?
A: Yes. Non-infectious vaginitis and yeast infections can occur without sexual activity.
Q: Are over-the-counter treatments effective?
A: For yeast infections, yes. However, misdiagnosis can lead to ineffective treatment, so consult a doctor if unsure.
Q: How long does it take to clear up?
A: With appropriate treatment, symptoms usually improve within a few days to a week.
Trusted Resources
For further reading, refer to:
Conclusion
Vaginitis is a manageable condition, especially when diagnosed early and treated correctly. By understanding its causes, recognizing symptoms, and following preventive measures, you can maintain optimal vaginal health and avoid recurrent infections. Always consult healthcare providers for the most accurate diagnosis and treatment plan.
